AI in pediatric cancer is transforming the landscape of treatment and monitoring for young patients battling this critical disease. Recent advancements in artificial intelligence tools have significantly enhanced the ability to predict pediatric cancer recurrence, particularly in cases involving brain tumors like gliomas. By analyzing longitudinal MRI scans, researchers can uncover patterns that indicate a potential relapse, leading to earlier interventions and improved patient outcomes. The integration of medical imaging AI with techniques like temporal learning serves to refine these predictions, shifting the focus from reactive care to proactive health management. As studies continue to reveal the potential of AI predicting cancer risks, the future of pediatric oncology looks increasingly hopeful for both patients and their families.
Artificial intelligence in the realm of childhood cancer is gaining traction and offers revolutionary methods for monitoring and predicting tumor behavior. Enhanced algorithms are now effective in assessing risks associated with pediatric tumor recurrence, particularly focusing on variations in glioma prognosis. These innovative approaches utilize advanced medical imaging technologies to track changes over time, allowing for a better understanding of a patient’s condition. Techniques such as longitudinal learning unveil insights that conventional methods often overlook, enabling healthcare providers to deliver personalized care plans. As we embrace this new era of technology in pediatric oncology, possibilities for improved treatment outcomes continue to expand.
Understanding Pediatric Cancer Recurrence
Pediatric cancer recurrence remains one of the most significant challenges faced by healthcare providers working with young patients. Recurrence can manifest months or even years after initial treatment, complicating the management of conditions like gliomas, a common type of pediatric brain tumor. These instances of relapse are not just a medical concern; they deeply affect the emotional and psychological well-being of children and their families. The anticipation and uncertainty surrounding follow-up procedures can create considerable stress, making the need for advanced predictive tools even more pressing.
As advancements in medical technology continue to evolve, understanding the factors that contribute to pediatric cancer recurrence is paramount. While many gliomas are considered curable through surgical interventions, their unpredictable nature means healthcare teams must remain vigilant. Predictive analytics tools, especially those enhanced by artificial intelligence (AI), offer a promising avenue for deciphering when and why recurrences might occur, allowing for proactive management strategies.
The Role of AI in Predicting Pediatric Cancer Outcomes
Artificial intelligence has revolutionized various sectors, and its role in predicting outcomes in pediatric oncology is increasingly recognized. AI-based tools, particularly those that utilize medical imaging and temporal learning methodologies, can analyze brain scans over time with remarkable accuracy. Research indicates that AI models can successfully interpret the progression and recurrence of cancers like gliomas by learning from a series of scans, making it an invaluable resource for predicting pediatric cancer outcomes.
The implications of AI in predicting the risk of cancer recurrence are profound. By analyzing patterns in imaging data collected over time, these AI tools can significantly enhance prognostic accuracy. In a clinical context, this means that healthcare providers can tailor their treatment plans more effectively, potentially leading to improved survival rates and enhanced quality of life for pediatric patients.
Temporal Learning: A Breakthrough in Medical Imaging
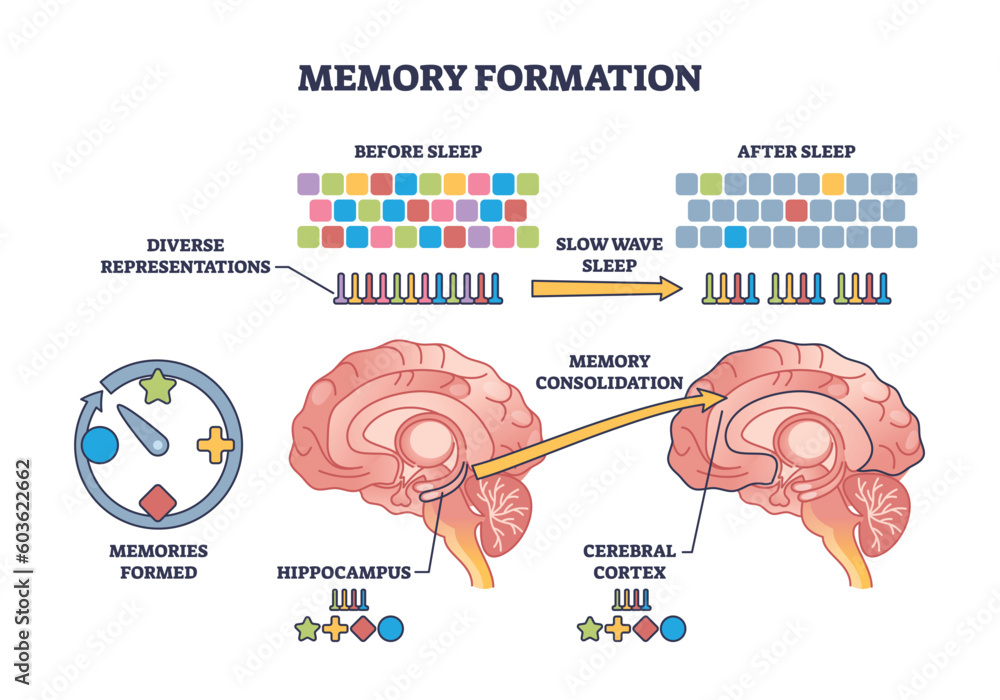
Temporal learning represents a significant advancement in the field of medical imaging, particularly when applied to pediatric cancer. This innovative approach involves training AI models to synthesize data from multiple scans taken over time, instead of relying solely on a single image. By utilizing this method, researchers have been able to provide insights into the subtle changes in brain tumors that may indicate a risk of recurrence long before traditional methods would detect any issues.
The incorporation of temporal learning into cancer prognosis not only improves accuracy but also reduces the burden of unnecessary imaging on patients. As studies suggest, the requirement of only four to six time-point images for optimal model performance illustrates the efficiency of this technique. This not only streamlines patient care but also enhances the overall effectiveness of monitoring treatment responses in pediatric oncology.
Leveraging Big Data for Pediatric Cancer Research
The integration of big data analytics into pediatric cancer research, particularly in the field of glyomas, marks a pivotal shift in how clinicians approach treatment and follow-up care. By aggregating vast datasets from thousands of MRI scans, researchers can uncover patterns and trends that inform the best practices for managing pediatric cancer. This data-driven approach not only enriches the understanding of how specific cancers behave over time but also illuminates the potential for personalized treatment strategies.
Furthermore, big data analytics enables researchers to identify at-risk populations among pediatric cancer patients more effectively. With robust, analytical AI tools at their disposal, healthcare providers can derive insights that lead to earlier interventions, thereby enhancing overall prognosis and long-term outcomes. The insights gained from big data analysis actively contribute to the refinement of clinical guidelines and inform future research directions.
Challenges of AI Implementation in Pediatric Oncology
Despite its promising potential, the application of AI within pediatric oncology is not without its challenges. One major hurdle is ensuring that AI tools are validated across diverse clinical settings, given the variability in patient populations and imaging techniques. Furthermore, there is an inherent need for transparency—in how AI systems arrive at their predictions and decisions—for healthcare providers to trust these novel tools.
Moreover, there are ethical implications regarding data privacy and the potential for bias in AI algorithms. Clinicians must be adequately trained in understanding AI outputs to bridge the gap between traditional practices and modern technological advancements in pediatric cancer care. Addressing these challenges is vital to ensure that AI becomes an effective ally in the ongoing fight against pediatric cancers.
The Future of AI in Predicting Cancer Therapy Responses
Looking ahead, the future of AI in predicting responses to cancer therapy holds great promise for pediatric oncology. AI tools that utilize advanced machine learning techniques have the potential to analyze not just imaging data, but also genetic and biochemical markers, providing a comprehensive picture of how each child’s cancer might respond to various treatment modalities. This multifaceted analysis paves the way for precision medicine in pediatric oncology, tailoring treatments to individual patient needs.
In conclusion, as researchers continue to refine AI methodologies and harness the power of big data, the integration of these technologies into clinical practice could lead to significant improvements in predicting therapy responses. With ongoing studies focused on gliomas and other pediatric cancers, the hope is that these advancements will enhance treatment efficacy and ultimately save more young lives.
Understanding the Prognosis of Pediatric Gliomas
Prognosis in pediatric gliomas can vary widely, depending on several factors, including tumor grade, location, and the patient’s age. High-grade gliomas, in particular, present a challenging landscape due to their aggressive nature and high risk of recurrence. The complexity of these tumors necessitates personalized approaches to treatment and vigilant monitoring to enhance patient outcomes. Thus, accurate prognostic tools that leverage AI and big data can transform how outcomes are assessed.
Understanding prognosis is critical not only for tailoring individual treatment plans but also for informing families about their child’s journey through cancer. AI-powered tools can provide insights that traditional methods may overlook, thereby fostering more accurate conversations between healthcare providers and families regarding expected outcomes and potential treatment trajectories.
Integrating AI into Pediatric Cancer Care Practices
Integrating AI into pediatric cancer care practices requires a comprehensive approach involving healthcare providers, technical experts, and families. This integration process begins with educating oncologists and radiologists on the capabilities and limitations of AI tools, ensuring that they can incorporate these technologies into their workflow seamlessly. As AI becomes part of the oncology toolkit, it holds the potential to revolutionize patient monitoring and treatment planning.
Collaboration between AI developers and healthcare institutions is essential in customizing algorithms that meet the unique needs of pediatric oncology. As these partnerships evolve, the focus must remain on improving patient care, with the ultimate goal being to develop predictive models that enhance early intervention strategies, reduce stress from frequent imaging, and streamline the family experience throughout the treatment journey.
Advancing Research Through AI in Pediatric Cancer
The role of AI in advancing research in pediatric cancer is increasingly becoming evident. With the ability to process vast amounts of data quickly and identify patterns that would be impossible for human researchers to detect, AI is revolutionizing the landscape of oncology research. The ongoing study of pediatric gliomas through AI tools showcases how effective data utilization can lead to groundbreaking discoveries that inform clinical practice.
Moreover, AI’s predictive capabilities can assist in identifying breakthrough therapies by analyzing responses to current treatments and patient demographics. As researchers continue to explore the integration of AI into pediatric oncology, we can expect to see significant improvements in how quickly new therapies are developed, tested, and brought to clinical use, ultimately benefiting countless children and their families affected by cancer.
Frequently Asked Questions
How is AI being utilized in predicting pediatric cancer recurrence?
AI is significantly improving predictions of pediatric cancer recurrence, particularly in patients with gliomas. Recent studies have shown that AI tools can analyze multiple MRI scans over time, leading to more accurate risk assessments than traditional methods. This advanced approach helps identify children who are at higher risk of relapse, allowing for timely and tailored interventions.
What role does temporal learning play in AI predicting cancer in pediatric patients?
Temporal learning is a groundbreaking technique in AI that enhances the prediction capabilities for pediatric cancer recurrence. By sequencing post-surgery MRI scans in chronological order, AI models can learn to recognize subtle changes in the patient’s condition over time. This method has proven to increase accuracy in predicting recurrence of both low- and high-grade gliomas, significantly improving patient outcomes.
Can medical imaging AI improve prognosis for gliomas in children?
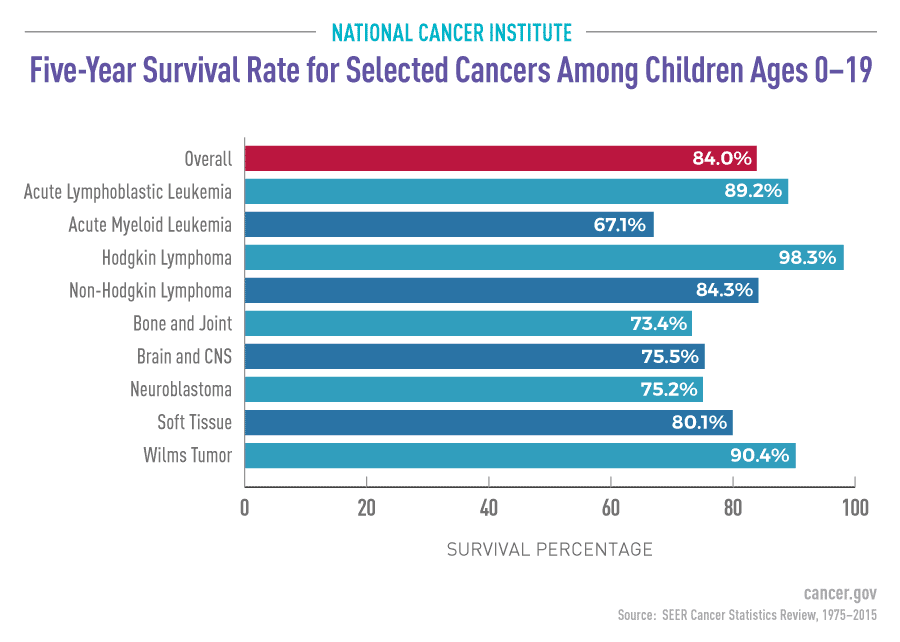
Yes, medical imaging AI plays a critical role in enhancing the prognosis for pediatric patients with gliomas. By using AI to analyze multiple brain scans, doctors can achieve a prognosis that is more precise, with recent studies reporting prediction accuracies of 75-89 percent. This high level of accuracy is crucial for determining the appropriate follow-up care and intervention for at-risk patients.
What advancements in AI predicting cancer could impact pediatric oncology?
Advancements in AI predicting cancer, particularly with methods like temporal learning, could significantly impact pediatric oncology by providing earlier and more reliable assessments of recurrence risk. This leads to the potential for customized treatment approaches, reducing unnecessary imaging for low-risk patients while ensuring closer monitoring for those identified as high-risk, thereby optimizing care.
How does AI enhance the analysis of medical imaging for pediatric cancer patients?
AI enhances the analysis of medical imaging for pediatric cancer patients by employing algorithms that learn from longitudinal data. In pediatric cancer cases, such as gliomas, AI can process and interpret multiple MRI scans over time, enabling it to detect subtle changes that may indicate relapse. This capability surpasses traditional single-scan assessments, allowing for proactive management of the child’s health.
What are the future implications of AI in managing pediatric cancer risk?
The future implications of AI in managing pediatric cancer risk are substantial. With ongoing research and clinical trials, AI tools promise to refine our understanding of cancer recurrence in pediatric patients. The ability to predict who is at highest risk for relapse can lead to more personalized treatment plans, potentially improving survival rates and quality of life for young cancer patients.
| Key Point | Details |
|---|---|
| AI Tool Prediction | AI predicts relapse risk in pediatric cancer patients more accurately than traditional methods. |
| Temporal Learning Technique | AI model uses data from multiple brain scans taken over time to predict cancer recurrence. |
| Research Impact | The study aims to improve patient care by identifying high-risk patients early. |
| Study Collaboration | Conducted by researchers from Mass General Brigham, Boston Children’s Hospital, and Dana-Farber. |
| Prediction Accuracy | Temporal learning showed prediction accuracy of 75-89%, a significant improvement over single image analysis (50%). |
Summary
AI in pediatric cancer is revolutionizing the way we predict and manage the risk of relapse in patients. By leveraging advanced AI tools that analyze multiple brain scans, researchers have demonstrated a higher accuracy in predicting the risk of recurrence in pediatric gliomas compared to traditional methods. This enhanced predictive capability not only offers potential improvements in patient care but also seeks to reduce the burden of frequent MRIs on families. As this research progresses, it holds the promise to significantly enhance the treatment and management of pediatric cancer.